14. The Anchor
There are many reasons why we get things wrong. This is a story about one of them.
‘Morning, guys.’ Jax greeted us at the cafeteria. ‘How’s everything?’
We were all there getting a quick breakfast before rounds. Peter, Jax, Kate and I. It was going to be an easy day, I thought to myself. All my patients had diagnoses and everything seemed to be going the right way. And that’s why I failed.
Rounds started and Kate went first presenting her patients. After she finished, I started with mine.
‘Mr. Porter is a 51-year-old male with a previous history of diabetes and peripheral neuropathy who was admitted to the hospital due to right hip pain after falling from his own height. His imaging report showed a femur fracture on top of a destructive lesion with sclerotic margins. He also has mild proteinuria and elevated creatinine.’
I continued describing his labs and answered a few of Dr. Rivers's questions.
‘Therefore I believe he has Multiple Myeloma and we should order protein electrophoresis with immunofixation. He also awaits surgery with the ortho team.’
Dr. Rivers was silent for a while.
‘Ok, Dr. Diaz. But what else could it be?’ I didn’t know what to say. ‘That is indeed a good hypothesis, but it doesn't fit perfectly, right? You said he has no anemia. How is his calcium?’
‘Normal.’ I said.
‘Right. Besides, if I am remembering it correctly the lesion in his bone is sclerotic, which is usually not the case in Multiple Myeloma.’ I nodded. I hadn't thought about that. ‘So maybe we need to think of other possibilities while we wait for the results.’
We discussed the other patients but honestly, I didn’t pay much attention to them. All I could think of was the fact that I was so sure about Mr. Porter’s case that I couldn’t see the things that didn’t fit. I couldn’t wait for rounds to be over so I could go rethink his case.
As soon as it finished I ran off to see Mr. Porter. I decided I needed to review everything I knew about him.
‘Hey, Mr. Porter. Do you mind if I ask you a few extra questions and examine you again?’
‘Not at all!’ He smiled. ‘I have nothing to do all day in this hospital anyway.’
‘Do you remember the last time you were completely healthy?’ I had learned this question with one of my attendings from medical school.
‘Hum… I think I would have to say last year when my feet started tingling.’
‘Oh, I see. What about your diabetes?’
‘True, there’s that. I found out I had diabetes three years ago, but I have it under control with metformin. My HbA1c is always 6!’ He said proudly.
Another thing that didn’t fit. I had mechanically thought his peripheral neuropathy was due to diabetes, but a 3-year-history of well-controlled DM does not commonly cause end-organ damage like that. I couldn’t believe I had missed that.
‘And is there anything else bothering you?’
‘Well, my feet get swollen sometimes. And I feel like my skin is getting darker.’
He was right. I could see that on his physical. And most importantly, as I examined him again I noticed he had splenomegaly. I guess it's hard to find what you're not looking for.
So my new chat with Mr. Porter flooded me with information I didn’t know how to deal with, but at least I could see I had narrowed it down to Multiple Myeloma too fast, and my mind just dismissed other options.
Hyperpigmentation, edema, splenomegaly, pathological fracture, sclerotic bone lesion, peripheral neuropathy, kidney damage. It was too much. And it was hard to believe that all of this could be explained by one disease alone.
I went home still puzzled by his case. I tried to read a little about it but it was hard to search about all these symptoms together. I needed something more specific.
Not long after that, we had some new lab results. Serum immunofixation was consistent with monoclonal gammopathy, but his urine was negative for Bence-Jones protein.
I called Dr. Rivers to discuss the results and he helped me see a new path.
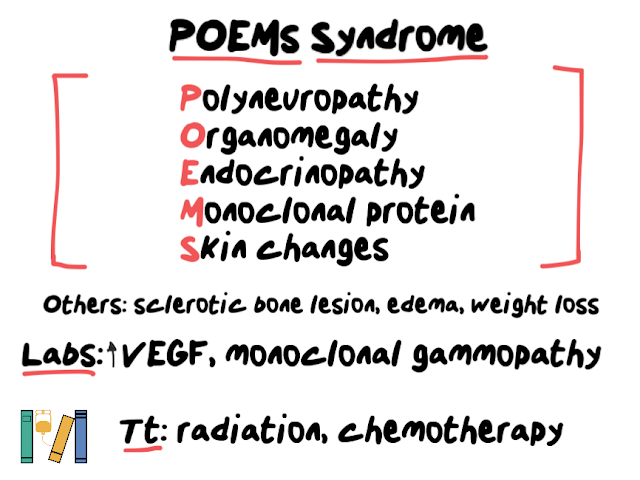
‘He has some kind of monoclonal gammopathy. Multiple Myeloma doesn’t really fit. Do you remember any other outside the Multiple Myeloma spectrum?’ I didn’t. ‘Try to study that. There is a syndrome called POEMS. I think it could fit his case, but I don’t remember all the criteria. Let me know what you find.’
I had never heard of that before, but now I had a clue of what to study. POEMS is an acronym and it stands for Polyneuropathy, Organomegaly, Endocrinopathy, Monoclonal protein, and Skin changes. Besides, there were many other criteria like edema and sclerotic bone lesions. Dr. Rivers was right after all.
We called Heme/Onc for a consult. Later that day, Dr. Rivers could see I was still upset about not getting Mr. Porter's case right.
‘That’s not the problem, Dr. Diaz. Multiple Myeloma is a good hypothesis. The problem is that you anchored yourself to that hypothesis and couldn’t see anything else.’
‘Anchoring bias.’ I scratched my head.
‘Exactly.’ He got up and patted me on the shoulder. ‘But don’t be too hard on yourself. It happens to all of us.’
…
Want to know more about POEMS Syndrome?
https://rarediseases.org/rare-diseases/poems-syndrome/
Want to read a real case of POEMS Syndrome?
https://casereports.bmj.com/content/2010/bcr.09.2010.3324
Clinical Board












No comments: